A Difficult Case of Pelvic Trauma
A patient is admitted after severe pelvic fracture from being struck by a vehicle. He has a severe rectal injury and undergoes a diverting colostomy and sigmoid colectomy down to the level of the rectum. He is discovered upon exploration to have a large intraperitoneal and extraperitoneal rupture of the bladder. These extraperitoneal lacerations were very complex and multiple and were repaired with full thickness sutures from the inside of the bladder. The bladder was thin anteriorly and some hernia mesh that has become incorporated into the retroperitoneal surface of the bladder at the level of the right side pubis.
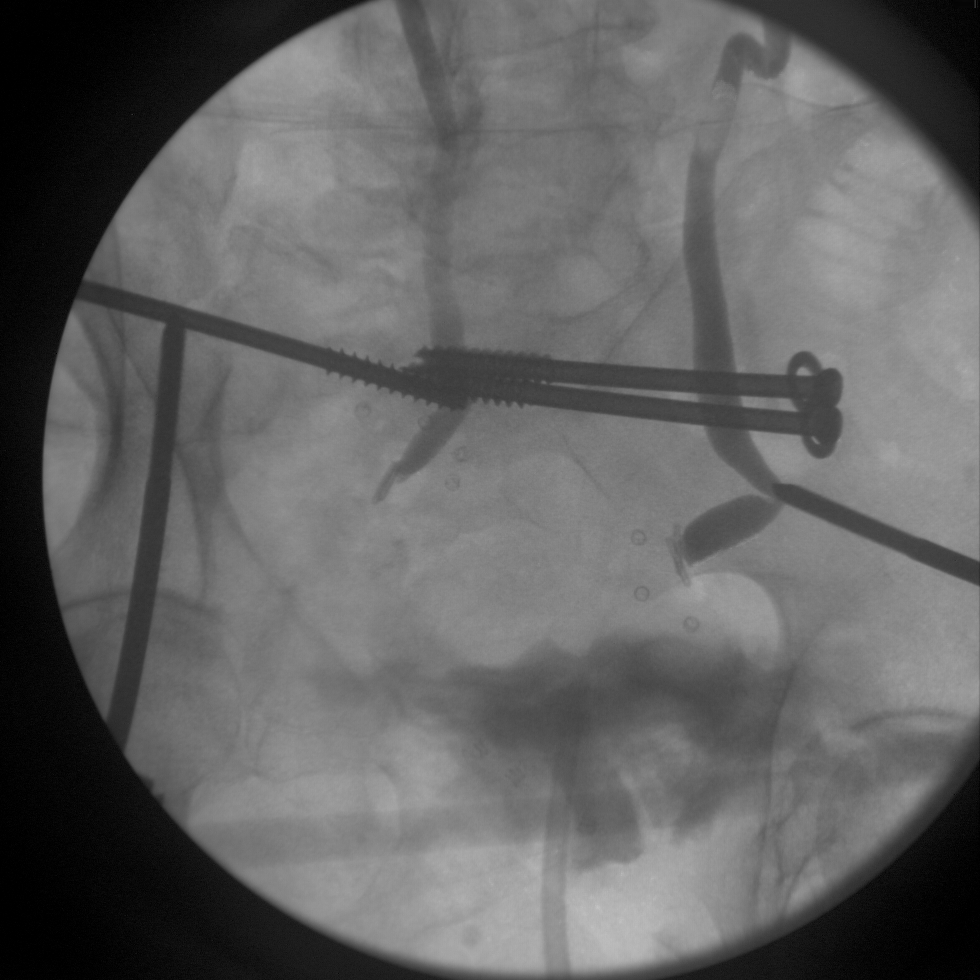
His repair remains water-tight but breaks down at about day 7 post injury. He begins to leak urine out of his external fixation pins. He has the following cystogram done.
Cystogram at day 7 after injury:

What are the choices now?
I proposed this question on Twitter recently. There were a few responses that mostly focused upon percutaneous drainage either with just percutaneous nephrostomy tubes, versus these combined with wire coil embolization of the ureters to prevent lower tract leakage. I was in agreement that the leakage down into the pelvis and around the exfix would likely lead to chronic fistula and the absolute need for urinary diversion if the patient was able to survive this problem at all.
I took a more direct route and explored the patient and tied off the ureters as low as I could go in the pelvic hematoma and then placed percutaneous nephrostomy tubes. I felt that absolute control of his urinary extravasation was essential to getting him to survive his pelvic fracture given how severe the leakage was and where is was coming out.
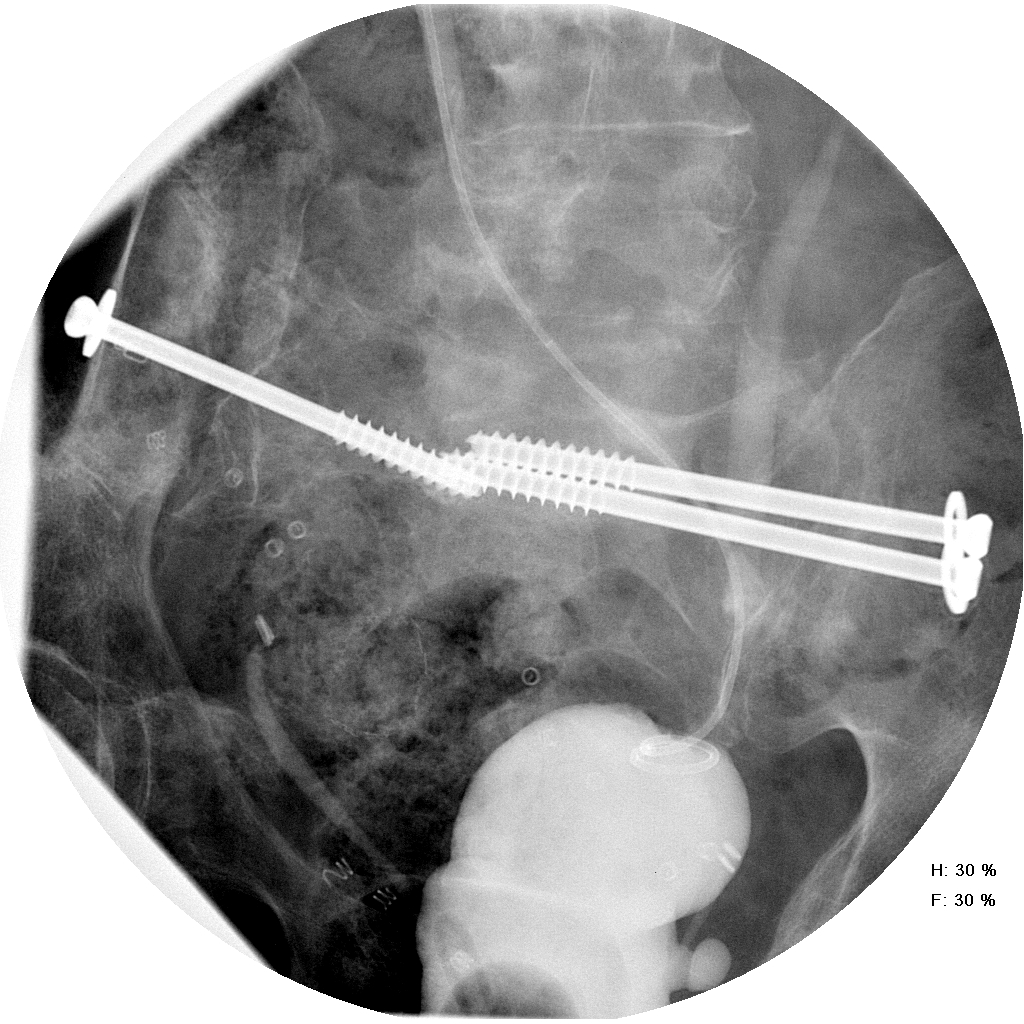
Subsequent antegrade nephrostogram at about 3 months showing relatively high ligation of the ureters.
At 9 months we took the patient back to the OR and he underwent colostomy takedown with rectal anastomosis. We reconstructed his urinary tract by grinding down the right side simphysis that pushed into the bladder space within the retroperitoneum. The bladder was completely healed in this location. We did a neocystotomy on the left side with a psoas hitch and a trans-uretero-ureterostomy from the right to the left so we could keep the pelvis clear for a good rectal anastomosis for the general surgeons. In addition we brought an omental flap based upon the left gastro-epiploic artery to overlay the anterior bladder and the area of simphyseal resection.
Post-op cystogram after TUU and psoas hitch with removal of large bony spicule on the right pubis.
Although this is unconventional approach and very aggressive, the patient has his bladder and the long-term the risk of urinary diversion and chronic unsalvageable pelvis would have been very high with chronic urinary fistula resulting from poor initial control of his urinary extravasation. The case reminds me of the surgical axiom about choices in surgery.
“Sometimes right, sometimes wrong, but never in doubt.”
This axiom is especially true in trauma care.
You can see a full case report on this case from Urology Case Reports here: http://www.urologycasereports.com/article/S2214-4420(14)00149-1/abstract
