Onabotulinum toxin A is a powerful drug that acts to temporarily paralyze muscles when it is locally injected. onabotulinum toxin A is known for its popular use in cosmetics, but it actually has far reaching medical applications. It is commonly used for diverse conditions like muscle spasticity, headaches, as well as the treatment of urinary incontinence.
Onabotulinum toxin A has been used to treat urinary incontinence for many years. It acts to decrease the muscular contractions of the bladder. These bladder “spasms” can arise from routine overactive bladder, which commonly occurs in women with aging or they can be more serious in patients with neurogenic bladder from neurologic disease or injury. Bladder spasticity has a lot of different names; it is also called overactive bladder, detrusor overactivity or hyperreflexia, and neurogenic bladder.
Onabotulinum toxin A needs to be injected into the muscle of the bladder. This is done in the clinic or operating room. First the bladder is flushed with a local anesthesia, via a catheter, that is allowed to thoroughly deaden the bladder. Then a scope is passed up the urethra (urine channel) into the bladder. A small needle is placed through the scope and many injections are made into the bladder designed to spread onabotulinum toxin A throughout the muscle of the bladder. Most patients tolerate this procedure well.
Onabotulinum toxin A begins to work at about 1 week, but the full effect of the medicine may take up to 2 weeks. Onabotulinum toxin A is not permanent and will last about 5-9 months in the bladder (average 6 months). Onabotulinum toxin A has a prolonged effect in the bladder compared to other muscles where it may only last a few months.
Onabotulinum toxin A acts to decrease the strength of the bladder’s natural contraction. It eliminates bladder spasm by this method. One potential side effect of this is urinary retention. In other words the onabotulinum toxin A works too well and patients cannot urinate on their own, or they have some residual urine in their bladder that does not pass with normal urination. Some residual urine does not cause much of a problem, but if this residual urine is high, or a patient cannot urinate a catheter has to be placed or a patient has to pass a catheter in order to drain their bladder. This complication is rare in patients with overactive bladder, because we limit the amount of onabotulinum toxin A we inject. If this problem occurs than a patient may have to catheterize themselves until the onabotulinum toxin A begins to wear off.
In patients with neurogenic bladder from conditions like multiple sclerosis or spinal cord injury we use much more onabotulinum toxin A than in a patient with overactive bladder. The reason for this is patients with neurogenic bladder often are dependant upon catheterization to start with. In these patients the goal is to inject enough onabotulinum toxin A so the bladder does not contract at all. This will eliminate leakage from bladder spasms and patients often are dry in between catheterizations.
There have been very few instances of onabotulinum toxin A ever causing systemic weakness when it is used in the bladder. This is a risk of onabotulinum toxin A therapy, but extremely uncommon.
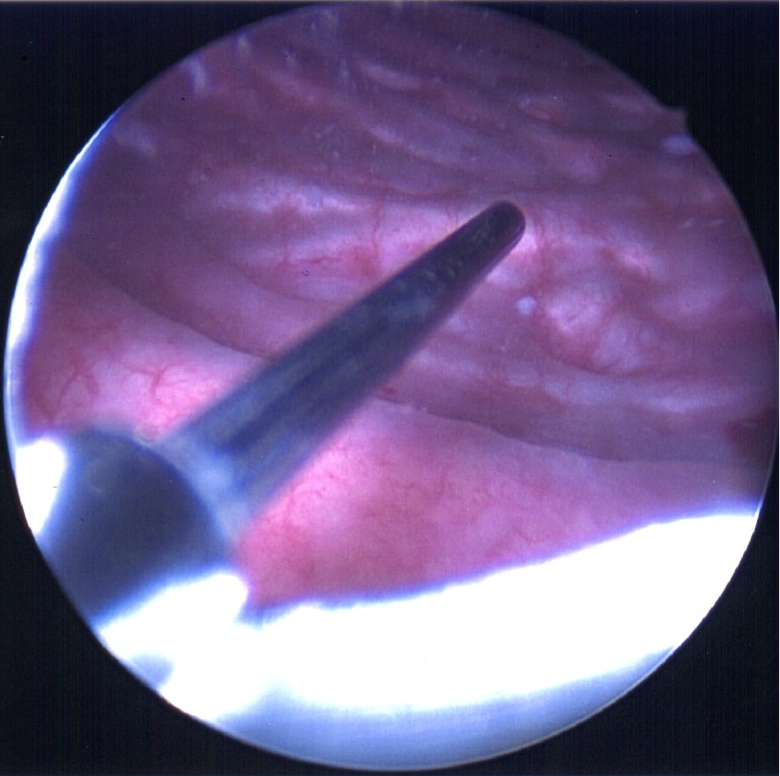
Figure: Injection of onabotulinum toxin A into the bladder wall from a small needle passed through a scope into the bladder.